Sexually Transmitted Infections (STIs)
What is a Sexually Transmitted Infection?
Have you been tested for chlamydia, gonorrhoea, HIV or syphilis by the sexual health department in Ayrshire? If yes, it is your responsibility to ensure you check your results. To get your results, call 01294 323226 – you will need your patient number “AN” followed by 8 digits. This service is available 24 hours a day 7 days a week once the results have been added to your patient record. This usually takes around 7 days.
STIs are passed from person to person via bodily fluids such as vaginal fluids, semen (cum), blood or even via genital to genital skin contact. Most do not survive for long on other surfaces but sex toys can also pass STIs from person to person. You can get some STIs from oral sex and some can affect your eyes.
Most STI’s can be easily treated with antibiotics, creams or anti-viral drugs, but not all can be cured. If you have had sex without a condom (unprotected sex) or if you experience condom failure (falls off or splits) there is a risk that you could have an STI. If this is left untreated there is a risk that you could pass this on to someone else. Practise safer sex by always using a condom for vaginal, anal or oral sex.
If you have been sexually active and start having symptoms (anything that has changed or is new for you) in your genital area you should call us on 01294 323226.
NOT ALL STI’S HAVE SYMPTOMS so we recommend you have testing whenever you have had sex with someone new. Our standard screening tests are for chlamydia, gonorrhoea, HIV and syphilis. It can take 2 weeks for chlamydia or gonorrhoea to show up on the tests, for HIV it’s 45 days and for syphilis it is 6 weeks.
What is Chlamydia?
Chlamydia is one of the most common STIs in the UK and is easily passed on during vaginal, anal and even oral sex. It can also be passed on by sharing sex toys. Most people have NO signs or symptoms. The only way to know is to get a test.
Chlamydia in the vagina can cause:-
- Pain or burning when peeing
- Unusual vaginal discharge. All people with a vagina have a discharge, but an unusual discharge may be thicker than normal, discoloured, or smelly
- Pain in your lower abdomen during or after sex
- Bleeding during or after sex or between periods
- Heavier periods.
Chlamydia in the penis can cause:-
- Pain or burning when peeing
- White, cloudy or watery discharge from tip of penis
- Pain or tenderness in testicles.
You can also get chlamydia in your rectum (bottom), throat or eyes.
If you have had unprotected sex or experienced condom failure contact your local sexual health department to get an appointment – click here or you can get a Chlamydia self-test kit from your local pharmacy (click here to find your nearest pharmacy). The test kit is either a swab from the vagina, throat or bottom or a urine sample. Your local pharmacist will take you through the process. This is a confidential service and NO correspondence will be sent to your home address unless you authorise this. All results go back to the pharmacist who will have arranged with you how you would like to receive the result.
Chlamydia in pregnancy
Chlamydia can be passed on to a baby during childbirth therefore pregnant people are offered an STI check during pregnancy by their ante-natal team. If you have chlamydia, you should arrange to have this treated, ensure you have a follow up test a few weeks later and another test 6 weeks before your due date.
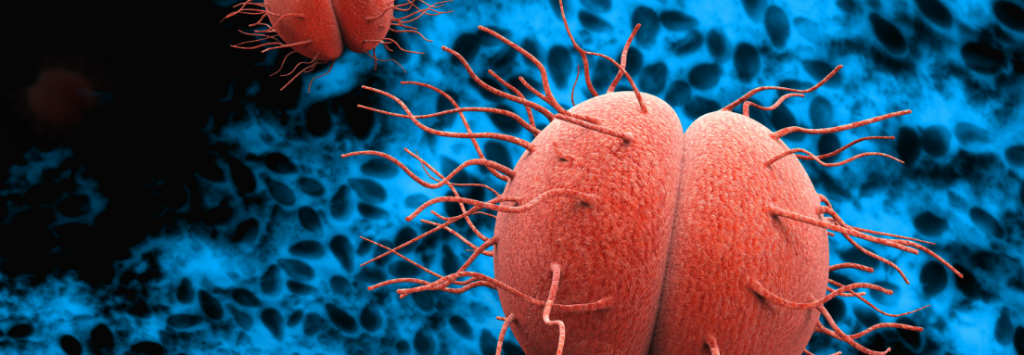
What is Gonorrhoea?
Gonorrhoea is an STI that is caused by a bacteria which can affect the penis, vagina, anus and eyes. Some people have NO signs; but for those that do, they might notice pain when passing urine (peeing) and/or a green or yellow discharge from the end of the penis or from their vagina. Gonorrhoea can cause long term complications including chronic pain, infertility and ectopic pregnancy due to damage to the reproductive organs.
If you think you may have gonorrhoea, make an appointment with your local sexual health clinic click here. You could also pick up a self-test kit from your local pharmacist (click here) who will talk you through the process. The test kit is either a swab from the vagina, throat or bottom or a urine sample. Your local pharmacist will take you through the process. This is a confidential service and NO correspondence will be sent to your home address unless you authorise this. All results go back to the pharmacist who will have arranged with you on how you would like to receive the result.
Gonorrhoea in pregnancy – gonorrhoea can cause premature delivery and can be passed on to a baby during childbirth therefore pregnant people are offered an STI check during pregnancy by their ante-natal team. If you have gonorrhoea, you should arrange to have this treated, ensure you have a follow up test a few weeks later and another test 6 weeks before your due date.
Gonorrhoea 4CMenB vaccine
The vaccine
The 4CMenB vaccine (usually used for preventing meningococcal infection) has been shown to be around 32-42% effective at protection against gonorrhoea.
On 10th November 2023 the Joint Committee on Vaccination and Immunisation (JCVI) recommended that the 4CMenB vaccine be offered to certain patient groups that would benefit most.
The vaccine is being used for an indication (clinical reason) that it was not originally designed for. This is called off-label use.
Free condoms still offer the best protection against gonorrhoea and other STIs.
Who will be offered the vaccine?
- Some Gay and Bisexual Men who have Sex with Men (GBMSM)
- Those with recent gonorrhoea infection or other bacterial STI
- Those with multiple partners or other risk factors
When will patients get the vaccine?
A process will now follow to decide how vaccines will be rolled out across Scotland. We hope to have more information soon and it will be publicised here as it emerges.
What is Herpes?
Herpes results from infection with the herpes simplex virus (HSV). It causes sores or blisters to form in or around the mouth or genitals, as well as other symptoms, you can catch HSV from someone with the cold sore virus on their lips or herpes on their genitals even when they have no symptoms and may be unaware they have this infection.
Genital herpes is mainly passed on during sex, through skin to skin contact with skin surfaces that carry the virus; such as pubic areas, penis, vagina, anus and mouth. Once the herpes virus gets into your system, as well as causing an initial reaction, it remains in your body permanently but not causing any harm. It may lie dormant like this for the rest of your life, however sometimes if your system is run down with a cold or flu you may experience another outbreak. The symptoms of herpes may begin with a tingling feeling or itching in the genital area, this may turn into several blisters and then turn into quite painful sores or ulcers. Passing urine (peeing) might be very uncomfortable. If you have symptoms of herpes you should start medication as soon as possible.
You can only be tested for the herpes virus when there is a visible “sore” present as a special swab needs to be taken at that time, you only need to have one positive test for herpes, it does not need to be done again if you have symptoms again. Although there is no cure for genital herpes, the symptoms can usually be controlled by using antiviral drugs. You should avoid having sex or close genital contact with someone if you or they have visible genital sores.
The medication to treat genital herpes does not cure the infection but it usually helps to reduce the symptoms and shorten the length of time it takes the sores to get better. This medication is available from your GP or sexual health clinic on prescription.
Useful links: Herpes Virus Association

What is Syphilis?
Syphilis is a bacterial infection that’s usually caught by having sex with someone who’s infected. The numbers of people who have caught syphilis continues to increase every year. Some people don’t notice any signs but the infection is in the body and can only be picked up with a test specifically for syphilis.
10 days – 6 weeks after initial infection some people notice single or multiple red ulcers/sores, which will heal after about 3-6 weeks. This is called a Chancre (pronounced “shanker”). They may or may not be painful. You might also notice swollen glands in the area near the sores. If syphilis is not treated at this stage, it will progress to the second stage.
The secondary stage occurs 1 week – 6 months after the first stage. And this may show as a rash on the skin often either on the palms of your hands, the soles of your feet or on your trunk (chest, stomach and back). There may also be swollen glands, headaches, aches and pains, hair loss, deafness or eye problems.
If left untreated at any stage, damage can be done to the brain, nervous system, bones, eyes and other organs. Syphilis can be easily spread through vaginal, anal and oral sex, as well as genital to genital skin contact with someone who already has syphilis. Syphilis may also be passed on through deep kissing if the infected partner has an ulcer (chancre) in their mouth.
The best protection against syphilis is to use a condom for all sexual activity including oral sex.
Syphilis can be transmitted to a foetus during pregnancy therefore every pregnant person in Ayrshire is routinely tested for syphilis early in their pregnancy.
Useful Links: Syphilis BASHH Leaflet, Syphilis in pregnancy
What are Genital Warts?
Genital warts are caused by certain variants of the human papillomavirus (HPV). Genital warts are small fleshy growths, lumps or bumps on the skin and appear on your genital anal and pubic area. Genital warts can be present on the skin without causing any visible warts, so it can be difficult to know when you acquired the virus. The virus can be passed on by close skin to skin contact, usually during sex with a partner who is already infected with genital warts virus. You do not need to have visible genital warts to pass the virus on to someone else.
If you think you have genital warts, it is important to speak to a health professional. They may want to look at the area you have noticed the changes; but this is up to you and is your decision. This might seem embarrassing for you but they are used to doing it. Genital warts, like other warts on the skin, will eventually resolve on their own. Treatment is an option if you want to speed up this process but often warts return within 6 months of successful treatment.
Anyone with lumps, bumps or sores on their genital region is recommended to have testing for chlamydia, gonorrhoea, HIV and syphilis.
RELATED PAGES

